The Sun's Trail -- How much is too much exposure to the sun?
by Sheri B. Doniger, DDS
Summertime approaches! It's especially true for those of us who live in the northern climes. We have visions of outdoor activities — playing sports, vacationing by the beach, or merely walking around enjoying nature's splendors. Sun exposure, at any time of the year, is unavoidable. During the summer, it can be inevitable. A suntan brings up an image of a healthy individual, as opposed to a pale face. This suntan is really the body's reaction to the injury caused by the sun's harmful radiation. We are all knowledgeable of the dangers of tanning and artificial tanning lights. We know to use SPF sunscreen, wear hats, and protective clothing.
But do we all follow these guidelines? Plastic surgery aside, we have one set of skin. Yes, it is constantly renewing but with the increased duration, frequency and intensity of exposures to the sun, photo aging occurs that can't be repaired. The skin appears wrinkled, mottled and dry. With today's focus on young, vibrant, healthy skin, the dangers of long-term sun exposure may be too much of a bad thing.
Skin cancer is definitely on the rise in the United States. It is the most common form of cancer. In 2002, more than 1 million cases of basal cell or squamous cell carcinoma have been diagnosed. Melanoma, which is the most malignant form of the disease, had over 50,000 cases reported. Since 1981, there has been a 7 percent increase in incidence of melanoma cases per year.
Exposure to the sun has been implicated as one of the major environmental factors of these cancers. Actually, it is the exposure to certain wavelengths of light that are the most dangerous. There are three types of UV rays: UVA, UVB, and UVC. Sunburn is caused by the ultraviolet rays, called UVA, which are the most abundant. The longer waves, UVB, will penetrate the skin to a deeper level. UVB rays have more absorption by the ozone layer than UVA. UVC radiation is the most harmful to skin, but it is completely absorbed by the ozone layer.
Sunlamps produce ultraviolet rays as well. The UVR received from the sunlamps may potentiate the amounts of sun exposure received during the course of a lifetime, hence making it more dangerous. The safety of these devices has been touted by the manufacturers, but the jury is still out.
Since the hole in the ozone layer was discovered over Antarctica in the early 1980s, there has been a decrease in the atmosphere's natural shielding affect of ultraviolet rays. Several major health problems have been associated with the overexposure to UV radiation aside from skin cancers. As anyone who has had a history of loving that summer tan will be able to tell you, premature aging of the skin is a latent side effect. Remember that tanning is a reaction of the body to protect itself against UV radiation. The skin reacts to this injury by increasing the number of melanin-producing cells. In addition, the sun will cause a reduction in the skin's elasticity. UVR can also induce a skin condition such as hives. This will appear as a generalized rash to the sun. In addition to skin cancers, which may not show up for many years after overexposure to the sun, ocular problems can occur. These include burns, cataracts, pterygium (tissue growth that can block vision) and macular degeneration. Immune suppression may occur, as exhibited by increased sensitivity to light, photoallergy and reactions to certain medications.
Sun exposure is not always a bad thing. Sunlight changes the precursor of Vitamin D in human skin from 7-dehydrocholesterol (provitamin D) to cholecalciferol.
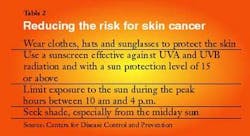
Protection from the sun year round is always a good idea. Using a SPF (sun protection factor) sunscreen with a minimum level of 15 will offer adequate protection for most individuals. Sunscreens scatter, absorb, and reflect the sun's rays. When thoroughly applied, these products will assist in preventing skin problems such as premature aging and actinic keratoses. Frequent applications may be necessary, depending on level of activity and amount of ambient sun exposure. Expiration dates should always be checked for product freshness.
To further block the harmful rays of the sun, eye protection that is recommended that will protect against at least 99 percent of UVA and UVB rays. Wrap-around glasses are preferred by experts. Protective clothing — such as wide brimmed hats, long-sleeved shirts and long pants — are recommended. When this is not possible, the diligent use of sunscreen should be implemented, in addition to seeking out shade.
The effects of ultraviolet radiation can be influenced by several non-genetic factors: the duration, the intensity, and the frequency of the exposures. Genetic factors include skin color (lighter skin more susceptible than darker skin), eye color, and familial history of previous cancer. There is one precancerous skin lesion and three cancerous skin lesions that we need to be aware due to sun exposure. (See Table 1)
Related lesions
Actinic keratosis is a precancerous skin lesion that is caused by UV damage from the sun. They are the most common sun-related growths and will affect approximately 60 percent people over the age of 40 who have experienced chronic sun exposure. Usually occurring in fair skinned individuals, the lesions appear as raised, dry, scaly, rough skin areas, or reddish brown papules or macules, varying in size from less than a millimeter to an inch in diameter. They can appear horny in texture, especially on the ears. Other regions affected will be the lips, face, hands, forearms, and neck. These lesions can present as non-healing ulcers.
The most aggressive form of actinic keratosis is actinic chelitis, which occurs on the lips and can evolve into squamous cell carcinoma. If this occurs, 20 percent will metastasize to other areas of the body. The lesions are slow growing, but if left untreated, may develop into squamous cell carcinoma. As with all the non-melanoma type skin lesions, there is a 95 percent positive prognosis if detected and treated early.
Basal cell carcinomas, which affect the basal layer of the epithelium, are the most common type of skin cancer, affecting 800,000 Americans each year. They appear as small, scaly bumps or nodules anywhere on the head and neck or as a non-healing ulcer. The ulcer may as a reddish or shiny patch, pink nodule, with rolled borders or scar-like. Tumors will appear with a higher prevalence (90 percent) on the exposed parts of the body, such as the scalp, ears, neck, shoulders, back, around the eyes or by the lips. Basal cell carcinomas are slow growing, usually benign, locally invasive but rarely metastasize. They can erode underlying bone if left untreated.
Squamous cell carcinoma is a malignant tumor affecting the squamous epithelium. It is the most common malignancy in the oral cavity and the second most common type of skin cancer. It can infiltrate via invasion through the basement membrane of the epithelium and metastasize. The lesion appears as an exophytic ulcer and can occur on the lips and the skin of the face. When affecting the lips, the vermillion border becomes mottled with fissures appearing. Solar chelitis may occur with epithelial dysplasia. The lesion is locally invasive. Although still a malignant lesion, the prognosis for squamous cell carcinoma of the lip is better than a lesion that presents intraorally.
Malignant melanomas are malignant tumors of melanocytes, causing approximately 75 percent of all deaths from skin cancer. Melanoma's incidence has increased in addition to the mortality rates. Approximately 7,400 Americans were estimated to die from melanoma in 2002. Patients most affected are usually over the age of 50, although it can be diagnosed as early as 20 years of age. The sixth most common type of cancer in men and seventh most common type of cancer in women, melanomas account for more than 80 percent of skin cancer deaths. It is the most common cancer in people younger than 30 years of age.
All melanomas evolve from melanocytes. Five types of melanoma exist. Superficial spreading melanomas (SSM) are slow spreading and usually arise from dysplastic nevi. They account for 70 percent of all lesions.
Nodular melanoma's (NM), is more aggressive than SSM, and usually do not begin as a nevus. Occurring on the head and neck areas, they arise during the middle decades of life and account for 15 to 30 percent of all melanomas.
Lentigo maligna melanoma (LMN) occur in older patients, are slow growing, and account for less than 10 percent of melanoma lesions. Acral lentiginous melanoma (ALM) occurs on the hands, feet and below the nail beds of affected individuals. These lesions make up 60 percent of all melanomas on darker skinned patients and only 2 to 8 percent of lighter skinned patients. Ocular melanomas will account for approximately 10 percent of the tumors. Their aggressiveness depends on the type of cell being mimicked.
Clinically, the tumors appear as a rapidly growing blue to black mass. The tumor is very aggressive and will metastasize. Four signs exist for differential diagnosis of these lesions from garden variety nevus. Melanomas are usually asymmetrical in shape, have border irregularities, exhibit a variety of colors within the same lesion and continue to grow or increase in diameter. This is usually described as the "ABCD rule."
Several risk factors increase the possibility of developing melanomas. Dysplastic nevi or moles tend to increase the risk factor for melanoma between 6 percent and 10 percent, depending on the age of the patient, family history and number of nevi present. Approximately 20 to 40 percent of melanomas arise from dysplastic nevi. Dysplastic nevi tend to be congenital and appear as larger than normal moles, usually appearing in areas that are normally covered from the sun, such as the scalp. Additional risk factors for melanoma include: family history of melanoma, light skinned/light haired individuals, immune suppression, a high number of normal nevi and excessive exposure to UVR with early multiple severe blistering sunburns.
New research is being conducted by the Department of Health and Human Service's National Toxicology Program Center for Phototoxicology on products that we apply to our skin. The NTP is based out of the National Institute of Environmental Health. The center is studying tattoos for the breakdown products of the inks utilized as well as alpha and beta hydroxyl acids that are in some of the anti-aging skin products. Their affects on UV radiation are being tested for phototoxicity and photocarcinogenicity. They will be testing for photoactivity or light sensitivity of drugs or substances and evaluate if they are a risk to potentially toxic or cancer risks in combination with UVR. This testing will offer insights to product safety.
We need to be increasingly aware of the variety of presentations these skin cancers exhibit while we conduct the extraoral examination. Prompt referral to an oral surgeon, dermatologist, or plastic surgeon may be life-saving, especially if the differential diagnosis includes a melanoma. We all want the look of physical well-being. But we need to keep the skin in healthy. Safe sun protocols, as listed in Table 2, should be practiced year round to keep our skin healthy for a longer time.
References
www.cdc.gov
www.fda.gov
www.epa.gov
www.skincarephysicians.com
www.melanoma-treatments.com/melanoma_types. html
www.skincancer.org/basal/index.html