Lichen planus pemphigoides: An autoimmune blistering disease
Lichen planus (LP) is classified as a cell-mediated immune-type mucocutaneous disorder. The name is derived from lichens, which are organisms that are found growing on rocks and trees with a plaquelike configuration. Some clinicians compare the appearance of these organisms to some of the various forms of oral lichen planus that have a white, lacelike presentation. One such type is the reticular pattern of lichen planus, also called Wickham striae because of the intricate white lines seen in this form.
There are various clinical presentations of true LP, and it may appear orally, on genitalia, and on the cutaneous areas of the body, especially the flexor surfaces of arms and legs. The lesions may be found in any mucosal lining such as the esophagus.
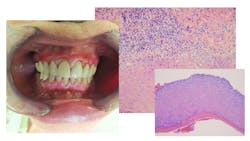
Lichen planus pemphigoides (LPP)1 is designated as a combination of lichen planus and bullous pemphigoid, or mucous membrane pemphigoid2 (figure 1).
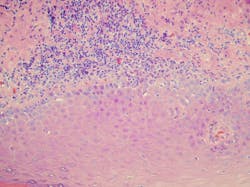
One of the theories behind LPP is that it initially starts as lichen planus. As the proteins from the basement membrane region become increasingly exposed as a result of chronic inflammation and damage, autoantibodies develop against one of these proteins (figures 2, 3).
LPP falls into the category of autoimmune blistering diseases. It is a rare occurrence, affecting 1:1,000,000, with most cases being idiopathic. The four types of blistering diseases that are described in the literature are pemphigus, pemphigoid, epidermolysis bullosa acquisita, and dermatitis herpetiformis. Some of these skin diseases and oral disorders may have similar overlapping features such as:
Pemphigoid: Subepithelial autoimmune blistering disease that targets the anchoring filaments. Biopsy will reveal a disconnect at the basement membrane. Multiple types exist within the category: mucous membrane pemphigoid, bullous pemphigoid, linear IGA disease (a subepidermal blistering disease), and pemphigoid gestationis (seen during pregnancy, exhibiting skin lesions and pruritis).
Pemphigus: Described as a threatening autoimmune blistering disease, with erythema and erosions. A positive Nikolsky sign is usually observed and can be present with pemphigoid as well. This involves using pressure on the normal-appearing tissue to determine if a blister forms.
Pemphigus typically exhibits autoantibodies against interepithelial adhesion molecules. Pemphigus is characterized by acantholytic intraepithelial blisters. There is loss of cell-to-cell adhesions of keratinocytes. Several types exist within this category such as pemphigus vulgaris and pemphigus foliaceus.
Lichen planus:2 LP has various types with some forms appearing plaquelike, erosive, or ulcerative, and—as mentioned previously—reticular and weblike.
A diagnosis is confirmed through a biopsy and the use of clinicopathologic correlation. The biopsy results are used to differentiate the above mentioned entities.3,4 With any of the skin diseases mentioned here, it is crucial to get a definitive diagnosis through a biopsy and adjunct immunofluorescence for confirmation.
Sometimes, medications can also produce a similar tissue appearance. This is called a lichenoid reaction. Changing or discontinuing the medication (with physician approval) generally produces a good result with the tissue returning to normal.
Recently, a case was reported of LPP in a patient who had received a black-ink tattoo and developed pruritic, violaceous papules/lesions distal to the tattoo site.5 The patient was treated with corticosteroids and antibiotics. Infection is listed as a possible etiologic factor for LPP along with reactions to medications.
The authors cautioned about this finding since tattoos continue to increase in the population and this may occur more often than reported. It is usually reported as an idiopathic condition.
Related: The venous lake: Oral pathology diagnosis helps rule out malignant possibilities
Possible etiology
The prevailing theory is that LPP results from epitope spreading, noted as spreading occurring because of damage to the basement membrane from lichenoid inflammation exposing antigens to autoreactive lymphocytes that develop an affinity for that area.6
For oral lesions, treatment usually involves corticosteroids such as dexamethasone solution, clobetasol, and combinations as necessary. Doxycycline may be indicated in some cases. Nystatin may be used, not for the treatment of LPP directly, but more so for sequelae of the steriod.
A very specific home care routine is needed with scaling and polishing every two to three months. Patients who have a mucosal disease are often recommended to use a manual toothbrush and a toothpaste with fewer additives and flavoring agents. Prophy jets are known to strip the epithelium, and in most patients with any chronic mucosal ulceration or disease, their use is not recommended.
Support for patients
The International Oral Lichen Planus Support Group (IOLPSG): Founded by Drs. Terry Rees and Nancy W. Burkhart in 1997, this site is through Texas A&M College of Dentistry and is supported through donations. Faculty from the Departments of Periodontics, Stomatology, and Oral Pathology participate periodically in assisting patients through the stomatology center at the dental school.
Drs. Nancy W. Burkhart and Paras B. Patel are cohosts of the site, providing information, referrals, and webinars to patients throughout the world. Many dental schools have oral medicine stomatology and oral pathology clinics that treat patients with mucosal diseases.
Over the years, the IOLPSG has obtained a list of providers who are well informed about lichen planus, along with other mucosal diseases. Many of those knowledgeable in this area are at dental schools throughout the world. We have found that patients may search for a definitive diagnosis for months and even years before obtaining the correct treatment for their disease.
The International Pemphigus and Pemphigoid Foundation has a website that can be accessed at pemphigus.org.
There are also special clinics such as the Center for Blistering Diseases in Boston that treat patients specifically with blistering disease states.
As always, continue to ask good questions and always listen to your patients.
References
- Otten JV, Hashimoto T, Hertl M, et al. Molecular diagnosis in autoimmune skin blistering conditions. Curr Mol Med. 2014;14(1):69-95.
- Allen C, Camisa C, Grimwood R. Lichen planus pemphigoides: report of a case with oral lesions. Oral Surg, Oral Med, Oral Pathol. 1987;63(2):184-188.
- Stoopler ET, Charmelo-Silva S, Bindakhil M, et al. Oral lichen planus pemphigoides: three cases of a rare entity. Am J Dermatopathol. 2020;42(6):467-469. doi:10.1097/DAD.0000000000001585
- Maceyko RF, Camisa WF, Bergfeld R, Valenzuela R. Oral and cutaneous oral lichen planus pemphigoides. J Am Acad Dermatol. 1992;27(5 Pt 2):889-892. doi:10.1016/0190-9622(92)70275-k
- Lim A, Tang PY, Oh CC. Lichen planus pemphigoides after body tattooing. J Cosmet Dermatol. 2020;19(11):3048-3052. doi:10.1111/jocd.13553
- Sultan A, Stojanov IJ, Lerman MA, et al. Oral lichen planus pemphigoides. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120:58-68.
Editor's note: This article appeared in the December 2021 print edition of RDH.
About the Author
Nancy W. Burkhart, EdD, MEd, BSDH, AAFAAOM
NANCY W. BURKHART, EdD, MEd, BSDH, AAFAAOM, is an adjunct professor in the Department of Periodontics-Stomatology, College of Dentistry, Texas A&M University, Dallas, Texas. She is founder and cohost of the International Oral Lichen Planus Support Group (dentistry.tamhsc.edu/olp/) and coauthor of General and Oral Pathology for the Dental Hygienist, now in its third edition. Dr. Burkhart is an academic affiliate fellow with the American Academy of Oral Medicine, where she also serves as chair of the Affiliate Fellowship Program Committee. She was awarded the Dental Professional of the Year in 2017 through the International Pemphigus and Pemphigoid Foundation, and she is a 2017 Sunstar/RDH Award of Distinction recipient. Her professional interests are in the areas of oral medicine and the relationship between oral and whole-body health, with a focus on mucosal disease and early oral cancer detection. Contact her at [email protected].