The venous lake: Oral pathology diagnosis helps rule out malignant possibilities
Your patient is Jennifer, a 44-year-old mother of three. You are treating her for the first time today in your office. While completing your health history, Jennifer mentions that she is thinking of having a dark area removed from her lower lip.
Jennifer says that she has had this removed previously by surgery (see Figure 1 representing view of venous lake as seen initially before removal a few years ago). However, the discoloration with obvious swelling has returned.
Figure 1: Previous image of the venous lake taken years before it was subsequently removed.
Figure 2: The current venous lake that has reoccurred. Note the bluish color with obvious bulging of venous lake that appears much larger in size than the initial lesion shown in Figure 1. Courtesy of Carol Perkins, BS, RDH, San Ramon, Calif.
She asks you what you believe may have caused this formation, and she requests information on what she has been told is a "venous lake" by her dermatologist. Since this is the first patient you have encountered with this type of entity, you quickly search your stored knowledge bank on the subject to provide some information to the patient. (See Figure 2 for the patient as seen currently in a dental office.)
A venous lake (VL) is usually described as a soft, blue/purple, compressible papule that is found on the sun-exposed surfaces of the lip, face, and ears. Other names associated with the venous lake are varicosity (varix), vascular formation, venous varix, venous lake tumor, venule, phlebectasis, and senile hemangioma of the lip. The venous lake is an acquired form of vascular ectasia or vascular dilatation.
Sun-exposed areas are more prone to this type of vascular damage since the sun over time will weaken the vascular walls in areas of the lips because of trauma and exposure to the thin layer of skin. This is why we do not see these in children. More commonly, they are seen in adults and aging populations who have significant histories of sun exposure. The average age group is over 50 years of age, and most are seen in males who are 65-plus years old because of the sun exposure accumulation of males who work outdoors.
The papule may continue to gain in size since the area is frequently traumatized, and it will continue to increase in size over time with each injury. Also, the varix in general may develop thrombosis, and they become much firmer in consistency and increase in size. The venous lake is usually within a range of 0.2-1cm in size. The lesions are asymptomatic and are usually removed for cosmetic reasons as they enlarge.
Treatment
The treatment procedures may include excision, electrosurgery, high-frequency electrical current, sclerotherapy, and cryosurgery. The venous lake can be treated with lasers such as the Dornier 940 or the 1064 Yag laser. Two to three treatments are usually standard.
Since this is often viewed as a cosmetic procedure, many insurance companies do not cover the costs. Even though the papule has been previously removed surgically, as in the case of the patient presented here, recurrence has been reported. Some negative reports related to surgery procedures include recurrence, lumpy tissue, and discoloration of the surrounding areas. The newer lasers appear to have better esthetic results than surgical removal and recurrence may be less reported.
Differential Diagnoses
The extraoral exam includes the sites where the venous lake is commonly reported such as the lip, the ears, and the face. It is not unusual for the dental professional to encounter someone who exhibits the venous lake, and the dentist/hygienist may receive questions from the patient regarding the diagnosis or treatment of these papules. Normally, referral to a dermatologist is the course of action. As mentioned in the treatment section, the papules can be removed with a laser in several procedures.
Why is a diagnosis important, if the lesion is benign?
The venous lake mimics a melanoma and also the basal cell carcinoma. Although these two entities have distinct characteristics at certain points in time, the bluish color may alert the clinician of a malignant possibility and promote consideration of these two entities. Other considerations include blue nevus, lentigo, and melanocytic nevi. Determining whether the lesion is vascular is the first step in determining the possible etiology.
Is it vascular?
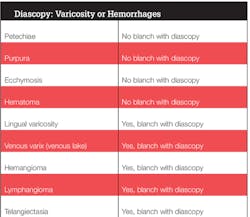
One procedure that is considered an "old standard" is to use a glass slide (or two, for more stability), placing it over the papule to determine if the flow of blood can be disrupted. The compression will cause the blood vessel to empty blood content. This procedure is referred to as diascopy. This disruption would provide some indication that it is more in line with a vascular lesion and not a fixed malignant growth. In addition, the appearance clinically of the basal cell carcinoma normally would exhibit crusting, rolled borders, and often a silvery hue in addition to the blue color. With any lesion, the only way to totally confirm the diagnosis (the gold standard) would be to view the tissue under the microscope.
Referral to a dermatologist is always considered the standard procedure (see related sidebar).
An Oral Medicine Perspective
The majority of patients will call the venous lake to the attention of their dental professional because of a concern for cancer. The second reason is because of the esthetic component. The discolored area may have increased in size, and the patient can no longer cover the papule's appearance with lipstick or make up.
When the papule has increased in size, trauma may become a component and the papule may bleed, crust, and become even more easily traumatized. The psychological component related to the venous lake is a prime consideration. Reassurance that the papule is not malignant is important and, after uncertain diagnosis, referral to a dermatologist is the accepted protocol.
As always, listen to your patients and continue to ask good questions! RDH
References
1. DeLong L, Burkhart NW. General and Oral Pathology for the Dental Hygienist. 2nd Ed. 2013; Wolters Kluwer Health: Lippincott Williams & Wilkins, Baltimore.
2. Colorado Skin and Vein. www.coloradoskinandvein.com/diagnoses/venous-lake/
3. The Vein Experts. www.veinexperts.org/veins/venous-words-simplified.asp
4. Senile Hemangioma of the lips. Mangal S, Padhiar B, Karia U, Shah BJ. Indian J Dermatol. 2014 Nov-Dec; 59(6):633. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4248532/
5. Weiss J, Weiss KD, Ross AL, Weiss E. (2014). A simplified minimally invasive technique for the treatment of venous lakes. Dermatology Online Journal, 20(1). doj_21257. Retrieved from: http://escholarship.org/uc/item/50q499fg
NANCY W. BURKHART, BSDH, EdD, is an adjunct associate professor in the department of periodontics/stomatology, Baylor College of Dentistry and the Texas A & M Health Science Center, Dallas. Dr. Burkhart is founder and cohost of the International Oral Lichen Planus Support Group (http://bcdwp.web.tamhsc.edu/iolpdallas/) and coauthor of General and Oral Pathology for the Dental Hygienist. She was a 2006 Crest/ADHA award winner. She is a 2012 Mentor of Distinction through Philips Oral Healthcare and PennWell Corp. Her website for seminars on mucosal diseases, oral cancer, and oral pathology topics is www.nancywburkhart.com. She can be contacted at [email protected].
About the Author
Nancy W. Burkhart, EdD, MEd, BSDH, AAFAAOM
NANCY W. BURKHART, EdD, MEd, BSDH, AAFAAOM, is an adjunct professor in the Department of Periodontics-Stomatology, College of Dentistry, Texas A&M University, Dallas, Texas. She is founder and cohost of the International Oral Lichen Planus Support Group (dentistry.tamhsc.edu/olp/) and coauthor of General and Oral Pathology for the Dental Hygienist, now in its third edition. Dr. Burkhart is an academic affiliate fellow with the American Academy of Oral Medicine, where she also serves as chair of the Affiliate Fellowship Program Committee. She was awarded the Dental Professional of the Year in 2017 through the International Pemphigus and Pemphigoid Foundation, and she is a 2017 Sunstar/RDH Award of Distinction recipient. Her professional interests are in the areas of oral medicine and the relationship between oral and whole-body health, with a focus on mucosal disease and early oral cancer detection. Contact her at [email protected].