Tailored treatment: Evaluation of salivary diagnostics
Rebecca Comstedt, BS, RDH
Recently, my daughter started feeling sick with a low-grade fever and sore throat. Ugh, sore throat! We had just had a positive strep test six months prior. This particular child is overdramatic about aches and pains, and a high-deductible insurance plan means doctor visits and tests are paid for out of pocket. I kept hoping it was just allergies and postnasal drip, but three days later, it was clear that her sore throat was not improving. I acknowledged that she needed a strep test.
My insurance plan had an option for a free telemedicine call with a doctor. But that did not solve the problem of the strep test. Not wanting to drop another $200, I had nothing to lose and tried the telemedicine option.
My daughter was a trouper as I struggled to get a good picture of her throat with my phone. The doctor came on, and we chatted for a bit about symptoms: low-grade fever, no cough, and recent history of a positive strep test. He agreed that her tonsils looked inflamed with white patches, and she had a strawberry appearance on her tongue. She checked all the boxes for strep, but there was no positive test. The doctor informed me that strep tests are available on Amazon—of course they are! I wished I had thought of that two days prior. The protocol for prescribing antibiotics is still a strep test, but given the circumstances, he was comfortable prescribing an antibiotic for her. Twelve hours and a $26 prescription later, my daughter was feeling remarkably better.
Why is the strep test so important? In a world of antibiotic resistance and microbiome awareness, we do not want to prescribe antibiotics unless absolutely necessary. In this case, strep throat left untreated can cause rheumatic fever, which, as we learned in hygiene school, can damage the heart valves.
As dental hygienists, we see bacterial infections all day long—decay, gingivitis, periodontitis—but unless we test for bacteria, we are only making assumptions about the etiology of the symptoms we see. If we undertreat a bacterial infection, the patient may experience systemic consequences (e.g., cardiovascular disease), inability to manage the condition, pain, and tooth loss. If we overtreat an infection, the patient may spend a great deal more money than necessary, antibiotics may be overused, and we may be wrongly treating the oral cavity as the source of the infection, when the periodontal disease may actually be a manifestation of a systemic disease. Until salivary testing becomes the standard of care, we are left making educated guesses to find the “Goldilocks” treatment for each patient—not too aggressive, not too conservative, but just the right amount of treatment.
We need to look at periodontal disease not only as dysbiosis of the oral microbiome, but also as a manifestation with nonbacterial etiologies. A variety of pathogens are responsible for periodontal disease, and they are vastly different in their pathogenicity, aggressiveness, and systemic considerations. If we treat periodontal disease the same way each time, we will not be successful in our treatment. Some patients will need antibiotics, antimicrobial rinses, and/or laser therapy, while others will not. No matter how amazing our clinical skills are, we cannot truly identify the etiology of our patients’ periodontal disease without testing.
Do we need to test everyone, even those who do not present with periodontal disease? Probably not. Just like individuals can be carriers of the strep bacteria without symptoms, we do not test or treat them if they are asymptomatic. The same may be true for periodontal pathogens. As long as patients’ microbiomes are in a state of balance and health and their bodies are able to keep any periodontal pathogens in check, there is no evidence that we need to proactively test everyone. However, there may come a time when the oral-systemic link is so strong and established that salivary testing becomes the standard of care to identify individuals at risk for particular systemic diseases.
Let’s take a look at the three most commonly used salivary tests. Rather than choosing just one, it may be advisable to carry two or three options in your office, as they offer different benefits.
OralDNA—This is a swish-and-spit test, in which the patient gargles and swishes with saline. The patient then spits into a funnel that is connected to a test tube. Results are available within a week. Results are paired with a recommendation for a systemic antibiotic. It is free to have the kits on hand; you only pay when you submit a sample. The cost to the office is around $99, plus shipping and handling. OralDNA offers a variety of other salivary tests, including one that identifies an individual’s genetic predisposition to periodontal disease (specifically the IL-6 gene) and one that screens for the HPV virus (a variety of strains). A one-hour webinar is available to learn more.
OraVital—This system uses paper points and swabs to collect bacteria from the tongue, throat, tonsils, and gingival pockets. The tests are sent to the OraVital lab for results. The test includes identification of S. mutans and C. albicans. The results are presented in an easy-to-read format, along with recommendations for the company’s proprietary rinses, which cost around $40–$120, depending on the rinse. Training to become certified in the company’s process is required, at a cost of around $1,000 for the whole team. The cost to submit a sample is $89, including shipping.
Hain Diagnostics—This company offers a paper point test that uses up to five paper points. These are placed into a collection tube for shipping. The easy-to-read result will come with a recommendation for systemic antibiotics that can be purchased at a local pharmacy. The cost for the kit is $109.
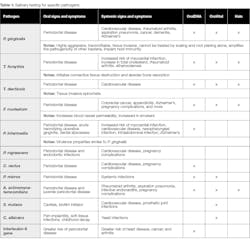
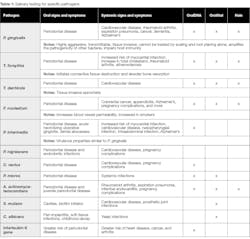
Salivary testing for specific pathogens
Let’s take a closer look at the specific pathogens, their systemic associations, and the salivary tests that will screen for the pathogens (table 1). A quick search on PubMed with the specific pathogen will show you research articles about the systemic associations. (Remember, association does not mean causation.)
Procedure codes
When implementing salivary testing in the office, it is important to submit the right code to insurance. D0417 is the code for “Collection and preparation of saliva sample for laboratory diagnostic testing.”
Controversy
Of course, there is controversy regarding the role of oral bacteria in the oral-systemic link. A June 2018 Journal of the American Dental Association article stated the following:
“Promoting the concept that prevention or treatment of oral disease reduces morbidity, prolongs survival, and reduces the cost of medical care is an attractive strategy for patient recruitment and to justify insurance coverage for oral health care. However, there remains a need for more convincing and higher quality evidence that oral health care actually has a measurable impact on specific systemic diseases before it can be claimed that attaining good oral health can prevent systemic diseases or conditions. It is premature to do otherwise.”1
The American Academy for Oral Systemic Health responded:
“It is a disservice to unknowing patients when practitioners neglect the mounting associations, causations, and level A evidence published in prominent medical journals [. . .] that infection in the mouth significantly contributes to medical conditions like Alzheimer’s disease, heart attacks, stroke, preterm births, diabetes, cancers, rheumatoid arthritis, and a host of other inflammatory conditions. [. . .] Major universities and medical institutions like the Cleveland Clinic are already changing their standard of care to incorporate the oral-systemic associations that research has uncovered. We have a responsibility not to overstate the relationship, but we are obligated to be informed and to inform our patients.”2
We do not want to use fearmongering to improve oral health, but if we utilize the right tools, we can present what we know, what we don’t know, and provide the best and most appropriate care for our patients.
References
1. Pihlstrom BL, Hodges JS, Michalowicz B, Wohlfahrt JC, Garcia RI. Promoting oral health care because of its possible effect on systemic health is premature and misleading. J Am Dent Assoc. 2018;149(6):401-403. doi.org/10.1016/j.adaj.2018.03.030.
2. Russo J, Estep S, Maples S, et al. AAOSH responds to JADA editorial that claims promoting oral-systemic connection is ‘premature and misleading.’ The American Academy for Oral Systemic Health website. https://aaosh.org/jada-response. Published June 13, 2018. Accessed September 13, 2018.
Rebecca Comstedt, BS, RDH,is a practicing clinical dental hygienist who lives in Westminster, Colorado. She is passionate about a holistic approach to oral health and the role dental hygienists play in improving total health. As founder of RDH Companion LLC, she supports other clinical hygienists by providing one place for leading hygiene educators to share current research, controversies, FAQs, and patient education. She is also a mom to three beautiful daughters.