A peri-implantitis patient will end up in your chair. Don’t panic, prepare!
Most seasoned dental hygienists remember the days when having a patient with an implant was a rare event. You and your coworkers would examine the x-ray with awe at the amazing technology that allowed oral surgeons to replace missing teeth with something that looked and felt so natural.
Today, implants are no longer a rarity. According to the American Academy of Implant Dentistry, about three million people in the US have dental implants, and another 500,000 implants are placed each year.1 While dental implants are an excellent replacement for missing teeth, they are not without risks. Problems can occur, including biologic and technical complications.
Numerous studies exist that have tracked implant failure. These studies show that many variables come into play for the long-term health of an implant. These include the following:
- type of implant used
- whether implants are loaded immediately or not
- type of restoration
- patient health status
Success rates are reported anywhere from 90% to 99.9% in the first five years.2 For the dental hygienist who treats implant patients for routine maintenance, there is much to be aware of when evaluating an implant for early signs of failure.
Causes of implant complications
What kind of events contribute to peri-implant complications? Upon acknowledging an ailing implant, the clinician can most often place the cause into a definite category. Let’s look at those categories.
Technical
The number of implants being placed has increased significantly over the past two decades, and the practitioners who place those implants have had varying degrees of clinical training. In the past—and even sometimes today—training has not comprehensively addressed how to manage complications, including ones caused by technical issues.
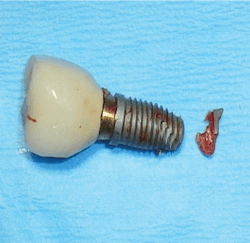
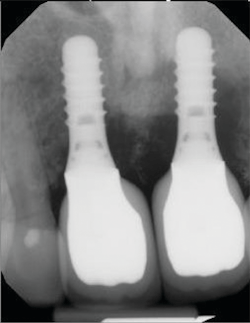
Technical issues include occlusal trauma, implant breakage, loosening of screws and abutments, and fracture, which can occur in screws, abutments, and/or porcelain. It should be emphasized that these are just a few of many potential problems (figure 1).
Esthetic
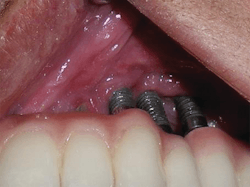
Both disease and corrective treatment can result in compromised esthetics. Frequently, implant esthetics are compromised due to exposed threads and abutments. This invites plaque and debris to harbor in the area.
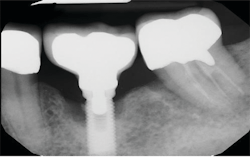
There are many choices in restorative options, and many result in highly esthetic final results. However, these restorations can make cleaning a difficult, if not impossible, challenge for the patient (figure 2).
Biologic
- Patients can be put in a vulnerable place if any of the following biologic risk factors are present:
- tobacco use
- alcohol consumption
- uncontrolled periodontitis
- history of periodontitis
- uncontrolled systemic diseases
- inability to perform adequate plaque removal
Studies comparing peri-implantitis occurrence on stable periodontal patients versus unstable maintenance patients show a higher rate of implant failure.3 We know that in individuals with a history of chronic periodontitis, the incidence of peri-implantitis can be four to five times higher than in individuals with no history of periodontitis.4
Peri-implantitis versus periodontitis
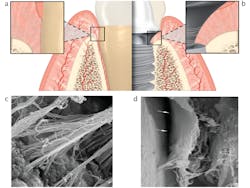
In order to treat peri-implantitis effectively, it can be helpful to understand the similarities and differences between it and periodontitis. For both conditions, the microbial composition of biofilm is similar—mixed and nonspecific. The sequence of immunopathological events in peri-implant infections are also similar to periodontal infections. However, peri-implantitis is marked by the following:
- more extensive inflammatory infiltrate and innate immune response
- greater severity of tissue destruction
- faster progression rate5
Why does inflammation attack implants differently than teeth? A lack of periodontal ligament around the implant limits the blood supply. Also, collagen fibers around the implant surface run parallel and not perpendicular, as the Sharpey’s fibers do to the cementum of the tooth (figure 3).6
Probing implants
It is interesting that, in spite of the extensive scientific research that has been done on this subject, many practitioners feel probing implants is harmful. But with the exception of the healing and integration phases, it is essential that hygienists probe implants. No scientific research exists to support the opinion that peri-implant probing may sever the soft tissue “seal” and jeopardize the integrity of an implant. Similarly, the notion of the need for plastic probes and implant scalers has been debunked.7 Periodontal probing is safe to do around implants, whether with metal or plastic, and should be done by the hygienist at each maintenance visit.
Peri-implant mucositis versus peri-implantitis
It is important to move quickly when peri-implantitis is suspected. Recognition of disease is imperative, and signs will vary depending on whether the condition exists as peri-implant mucositis or peri-implantitis. These two conditions can be compared to gingivitis and periodontitis in a natural tooth: diagnosing and treating peri-implant mucositis can prevent further development into peri-implantitis and implant failure.
Peri-implant mucositis
Peri-implant mucositis is reversible inflammation without bone loss. In this situation, there will be obvious redness, edema, bleeding on probing, and pseudopocketing—but again, no radiographic bone loss. This is why gentle probing and tissue evaluation must be done at each maintenance visit.
At the first sign of inflammation, the hygienist must set aside the time to inform the patient about the condition. Patient education must be a priority. At this crucial point, it is imperative that hygienists get out their mirrors and do some old-school oral hygiene instruction. Put the brush in the patient’s hand, study his or her home-care routine, and target any shortcomings.
In addition to patient education, the restoration must be evaluated—is the shape conducive to cleaning? Is the fixed overdenture too tight against the tissue for interdental aids to access? An occlusal analysis is also in order, as well as the fabrication of a bite guard if needed. Scaling and detoxification of the implant surface must be done immediately, but with a warning to the patient that there is a risk of postoperative recession once the infection clears.8
It is important to schedule a reevaluation appointment a few weeks later. If peri-implant health has not been achieved, a surgical or laser intervention must be considered.
Peri-implantitis
Peri-implantitis, when compared to peri-implant mucositis, is a more severe form of disease. It can be a result of untreated peri-implant mucositis. There is emerging evidence that the lack of annual supportive therapy in patients diagnosed with peri‐implant mucositis is associated with increased risk for conversion of peri-implant mucositis to peri‐implantitis.9 In one study, 18% of the patients complying with supportive therapy presented with peri‐implantitis after five years, while the corresponding proportion of patients who did not adhere to supportive therapy was 43.9%.4
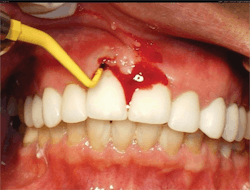
Symptoms of peri-implantitis may include bleeding on probing, deep probing depths, edema, redness, suppuration, and radiographic bone loss (figures 4 and 5).
The action steps to treatment are the same as for peri-implant mucositis, with the reevaluation from implant detoxifying determining whether surgery is necessary. Some studies suggest that nonsurgical treatment efforts work best in peri-implant mucositis, and that in the presence of peri-implantitis, surgical or laser intervention is the only option.10
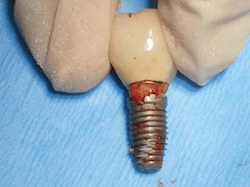
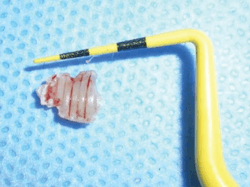
One of the most perplexing causes of peri-implantitis is residual cement being left behind unknowingly. The cement is often difficult to feel with an explorer and not always visible radiographically. This happens often enough that the problem has earned its own name, “cementitis,” and it can create an infection severe enough to cause the implant to fail (figures 6–8).
Solutions to prevent retained cement include raising the restorative cement line, using only radiopaque implant cements, or using screw-retained implants.
Nonsurgical treatment and professional maintenance
Just as in periodontitis in natural teeth, peri-implant mucositis is not curable. We can only get it under control and attempt to keep it there.
The first step when peri-implant mucositis is suspected is educating the patient about the following:
- proper home-care techniques
- the need for more frequent maintenance visits
- the truth about the risks if recommendations are not followed11
The more education that is done, the more likely the patient will comply with instructions.
In my office, many patients who come to us with failing implants think of their implants as “fake teeth.” They think the implants are somehow not really “theirs” and do not require careful plaque removal daily. Once told these implants are integrated into their own bone and susceptible to the same periodontal disease as a natural tooth, the reality of the situation hits.
Many denture patients who are not used to dental care inside their mouths (caring for their dentures only) receive a rude awakening once they realize the time-consuming work involved in caring for a fixed overdenture. Denture patients are also not used to maintenance visits every three to four months. Oftentimes denture patients do not even seek out regular dental visits for denture cleaning or oral cancer screenings. Visiting the office several times a year to have their implants cleaned and checked is a difficult routine to get accustomed to.
For all implant patients, reinforcement is necessary at all times. This is true whether patients are doing well with home care or not. For patients who are doing great at plaque removal, remind them that this is the reason for the good health and positive outlook for the longevity of their implants. For patients who are missing the mark on plaque removal, commend them on what they are doing right, and then continue to educate them and help them improve. Also, continue to recommend any crucial home-care aids and explain how to use them.
Let’s now look at some of those crucial home-care aids a little closer.
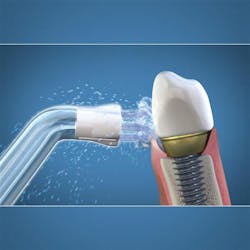
Water-irrigating device
Particularly useful for fixed overdentures or implant bridges, water-irrigating devices have improved in their ability to dislodge plaque and debris. Studies show water-irrigating devices are superior to string flossing.12
In particular, the Waterpik brand has established an important place in implant care with its line of various brush tips. Research supporting the benefits of water irrigators has been primarily done using the Waterpik water-flossing device. In a study conducted at Tufts University, people who used a water flosser with the Plaque Seeker tip reduced bleeding around implants twice as much as people who used string floss.13 These tips flex easily to navigate their way around implant prosthetics, often reaching areas that the patient cannot manage with other tools. Replacement Plaque Seeker tips are inexpensive, easy to obtain, and fit on all Waterpik models (figure 9).
Interdental brushes
A staple for home care in all periodontal patients, the interdental brush (bottle brush; figure 10) is crucial for the care of implant embrasures, especially when they are wide. Unlike a natural tooth with a wide platform above the furcations, posterior implants have a wide tooth perched on a narrow post. This creates two nooks that invite both plaque to harbor and food to impact. A solution is to insert the widest interproximal brush that will comfortably fit in the space. The brush not only provides tissue stimulation but also removes plaque and debris instantly. Dipping the brush in an antiseptic increases the benefit.
Toothbrush for fixed dentures
TePe manufactures a brush perfectly suited for accessing areas under prostheses. Formerly called Implacare, the brush is now called Universal Care (figure 11). Its soft bristles are arranged horizontally and adapt readily to the denture.
Professional care
There still exists a wide array of opinions among dental hygienists regarding implant maintenance instruments and techniques. Even the issue of probing is debated. But scientific research has been done extensively on the subject, and implant surgeons now recognize that much of what we thought in the past has been disproven.
Plastic versus metal scalers
In the past, the only safe scaler for an implant was thought to be made of plastic or having a plastic sheath placed over a metal ultrasonic tip. But these were not entirely safe due to plastic debris left behind and being ineffective for removing anything more than soft plaque from the implant. Today, titanium implant scalers that are safe and effective are available from most popular dental instrument companies. They come in different designs and can be sharpened.
Currently, there are no alternatives to plastic ultrasonic sheaths for performing the desirable ultrasonic cleaning. As hygienists, the goal of our preventive treatment is to clean without leaving roughness that may cause increased amounts of bacterial biofilm. A recent study showed that traditional stainless steel ultrasonic tips leave a rough surface, but that power level and pressure affect this greatly.14 Ultrasonic tips made of a copper alloy were shown in a study to be effective and as minimally influential on the titanium surface as plastic. However, these tips are not available commercially yet.15 A greater variety of ultrasonic tip materials needs to be tested and studied. Until that time, the conclusion of current studies seems to be that ultrasonic scalers with nonmetal tips are suitable for safe implant maintenance.
Polishing methods for implants have been studied, and the Airflow glycine powder air polisher (Hu-Friedy) is now considered the standard of care for safe polishing of titanium surfaces. There is also some evidence that bacterial colonization is inhibited using such devices.16 When we use a conventional prophy angle to polish exposed implants, it is suggested that we use a low-abrasion polishing paste (not medium- or coarse-grit) or plain toothpaste. For offices that do not have a glycine air polisher, this type of paste is recommended.
Final thoughts
Dental implants are marvels of modern dentistry and great replacements for missing teeth. But patients must be made aware that implants are susceptible to similar periodontal issues that natural teeth have, and often are attacked more aggressively.17 As conscientious dental hygienists, we want to do what is best for our patients, even if that means ending “what we have always done” in order to comply with the latest scientific research. It is not always easy educating patients (or employers) why you think your protocol may be out of date. Newly discovered treatment protocols can take years to catch on, but by using modern methods, you can feel confident. You will stand out among your peers as a prepared hygienist who stays on the cutting edge of treatment modalities.
References
1. Homepage. American Academy of Implant Dentistry website. https://www.aaid.com/index.html. Accessed June 19, 2019.
2. Jung RE, Zembic A, Pjetturson BE, et al. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow‐up of 5 years. Clin Oral Implants Res. 2012;23(6):2-21.
3. Pjetursson BE, Helbling C, Weber HP, et al. Peri‐implantitis susceptibility as it relates to periodontal therapy and supportive care. Clin Oral Implants Res. 2012;23(7):888-894.
4. Karoussis IK, Salvi GE, Heitz-Mayfield LJA, et al. Long-term implant prognosis in patients with and without a history of chronic periodontitis: A 10 year prospective cohort study of the ITI dental implant system. Clin Oral Implants Res. 2003;14(3):129-139.
5. Heitz-Mayfield LJ, Lang NP. Comparative biology of chronic and aggressive periodontitis vs. peri-implantitis. Periodontology 2000. 2010;53(1):167-181.
6. Froum S, Kurtzman G. Top 5 anatomical differences between dental implants and teeth that influence treatment outcomes. Perio-Implant Advisory website. https://www.perioimplantadvisory.com/clinical-tips/periodontal-complications/article/16412223/top-5-anatomical-differences-between-dental-implants-and-teeth-that-influence-treatment-outcomes. Published September 13, 2017. Accessed June 17, 2019.
7. Shah R, Talati M, Mitra D, et al. Implant maintenance: A new protocol. Int J Adv Res Tech. 2017;2(11):49-51.
8. Froum S. Peri-implant mucositis: Are you a clairvoyant or a charlatan? Perio-Implant Advisory website. https://www.perioimplantadvisory.com/clinical-tips/article/16411574/periimplant-mucositis-are-you-a-clairvoyant-or-a-charlatan. Published March 15, 2016. Accessed June 17, 2019.
9. Costa FO, Takenaka‐Martinez S, Cota LO, et al. Peri‐implant disease in subjects with and without preventive maintenance: a 5‐year follow‐up. J Clin Periodontol. 2012;39(2):173-183.
10. Renvert S, Roos‐Jansåker A, Claffey N. Non‐surgical treatment of peri‐implant mucositis and peri‐implantitis: a literature review. J Clin Periodontol. 2008;35(8):305-315.
11. Suárez-López DAF, Yu SH, Wang HL. Non-surgical therapy for peri-implant diseases: A systematic review. J Oral Maxillofac Res. 2016;7(3):e13.
12. Goyal CR, Lyle DM, Qaqish JG, et al. Evaluation of the plaque removal efficacy of a water flosser compared to string floss in adults after a single use. J Clin Dent. 2013;24(2):37-42.
13. Jahn CA. Enhancing dental implant health by water flossing with the Plaque Seeker tip. DentistryIQ website. https://www.dentistryiq.com/products/article/16365648/enhancing-dental-implant-health-by-water-flossing-with-the-plaque-seeker-tip. Published March 14, 2017.
14. Mann M, Parmar D, Walmsley AD, et al. Effect of plastic-covered ultrasonic scalers on titanium implant surfaces. Clin Oral Implants Res. 2012;23(1):76-82.
15. Baek SH, Shon WJ, Bae KS, et al. Evaluation of the safety and efficiency of novel metallic ultrasonic scaler tip on titanium surfaces. Clin Oral Implants Res. 2012;23(11):1269-1274.
16. Di Salle A, Spagnuolo G, Conte R, et al. Effects of various prophylactic procedures on titanium surfaces and biofilm formation. J Periodontal Implant Sci. 2018;48(6):373-382.
17. Pjetursson BE, Heimisdottir K. Dental implants–are they better than natural teeth? Eur J Oral Sci. 2018;126(1):81-87.
About the Author

Linda Rhoades, BS, RDH
Linda Rhoades, BS, RDH, has been a dental hygienist for 42 years and enjoys writing, speaking, and mentoring her fellow dental hygienists. She was the 2021 recipient of the Irene Newman award from ADHA, and is author of the book Irene Newman: The World’s First Dental Hygienist.