Sarcopenia
As I settled in to watch Oscar Night - that dazzling evening when the achievement awards are presented to motion picture celebrities - my attention was drawn to a comment by Dustin Hoffman: “If it ain’t broke, don’t fix it.” I understand the familiar saying to mean that if something works well, there’s no reason to change it. But that sentiment certainly does not ring true for many dental hygienists, especially those of us who are constantly reinventing ourselves and redefining our growing profession. I’m forever trying to dream up new topics for my column and articles, because I know that I, too, get tired of reading the same boring stuff over and over again.
A few years ago, I met a dentist who immediately struck me as totally unlike any dentist I’d ever met before ... and that, in itself, can be a good or bad thing! Hisname is Dr. Frank Varon, and he has a general/oral medicine practice with a strong focus in diabetes care in Omaha, Neb. Dr. Varon grew up with a father who was an endocrinologist. His influence stirred in Dr. Varon a desire to treat his patients not as just a set of teeth to work on, but as intricate human beings with body systems that need to work in sync. Dr. Varon encouraged me to broaden my horizons and submit an abstract to the CDC Diabetes Translation Conference in 2005. Never in a million years did I think I would be presenting a paper at such a meeting! Tackling a new topic that I had never focused on before, I completely immersed myself in the subject and have come to love it.
Dr. Varon and I chat on the phone occasionally, and we e-mail each other from time to time. His jokes are often funny and worthy of a chuckle, like his latest observation about “giving topless grandmothers a lift.” Frank believes very strongly that many dentists and dental hygienists often forget about the relationship between oral health and general health, and the Surgeon General’s comments about the mouth being a mirror for general health and well-being.1
Dr. Varon has some genuine concerns about the direction and focus of periodontal assessments that only take into account the measurement of past disease activity, which is what we get when probing to measure clinical attachment loss. His interest in risk assessment includes systemic health problems that might influence the status of oral health. Here’s a good example of the main point Frank is trying to make.
Sarcopenia is a decrease in muscle mass due to normal aging. It rears its ugly head in the fourth decade of life at about age 45, when muscle mass begins to decline at a rate of about 1 percent per year. As patients age, they become frail and weak. This gradual loss has been attributed to protein deficiency, lack of exercise, and increased fragility.3 To learn more about sarcopenia, there’s a reputable research agency at Tufts University where researchers have been studying the ailment since 1988. Researchers there have repeatedly shown the safety and effectiveness of resistance (or strength) training in reversing sarcopenia and frailty in the elderly.
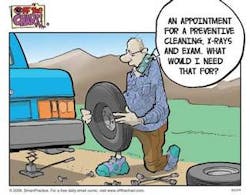
Most of us have noticed that as our patients age, their manual dexterity decreases. We’ve all worked with geriatric patients who tell us that they’re using that special powerbrush we recommended for a full two minutes. They also emphasize that they’re flossing like there’s no tomorrow, but when we peek inside their mouths, we’re shocked by the presence of thick, cheesy, gross debris along the gingival margin that makes us want to return to school to earn a new degree. Is the older patient’s periodontal condition worsening because of a heightened inflammatory response, or is it simply because of an overabundance of pathogenic bacteria due to poor home care?
Now, let’s take this discussion a step further. The U.S. population is graying, and as the baby boomers age, the older population will be larger than ever. Some 84 million of us born between 1946 and 1964 make up one-third of the U.S. population. This group is highly visible and extraordinarily influential in shaping our culture. With these large increases in the population of older adults come increasing numbers of people suffering from chronic diseases, and many don’t get timely medical and dental care. They sometimes don’t take their medicine as prescribed, and they are a complex bunch to treat medically and dentally in our current U.S. health-care delivery system.
One cardinal complication of many of these boomer-age chronic diseases involves musculoskeletal disorders. These disorders primarily affect the skeletal muscle of the body, including the arms, wrists, and hands.2 In our population of patients with diabetes, for example, why aren’t we assessing hand function when we conduct clinical trials on older adults with periodontitis? Numerous hand disorders (syndromes) are very common in individuals with diabetes and other systemic diseases, and they can impair oral hygiene skill performance. If you doubt what I’m reporting here, google a most intriguing Web site at Hand University (www.handuniversity.com) to learn more about the oodles of hand, wrist, and elbow dysfunctions that specialists see every day. Again, why are we not conducting more research in dental hygiene to discover new techniques and devices to improve the oral hygiene efforts of these individuals?
Shouldn’t we, as periodontal therapists, be focusing on grip-and-pinch strength testing in private and public health settings and continually researching new ways to improve oral hygiene in the older population? Why haven’t we begun to focus on musculoskeletal problems in an aging population as a measurable risk factor for dental caries and periodontal diseases?
The frailty of the aging boomer population continues to emerge as a significant public health problem because it impairs mobility, thus interfering with the quality of life and increasing the risk of falls. Individuals with sarcopenia are also sometimes restricted in the use of health-care resources, and adaptations of dental facilities to enhance autonomy by elders has not yet been given priority status.
In the performance of daily oral hygiene skills, perhaps we should look at behavior modeling and try to identify and analyze requirements that must be satisfied for oral hygiene procedures to be reliably, effectively, and safely performed. Now that we are facing a boomer explosion of unprecedented proportions, perhaps now is the time to focus on this important issue.
Sarcopenia is well-documented in the medical literature but has never been written about in the dental literature. Dr. Varon poses a very important question to our profession on this issue, and he suggested I introduce the topic to the dental hygiene community. Along these lines, he also asked me a question, which I believe we should think about long and hard: “Do you see how sarcopenia might impact the oral health of our patients as they age or suffer from chronic diseases?”
In addition to sarcopenia, arthritis is the leading cause of disability in older adults. It can severely limit daily activities such as the performance of oral hygiene care. Strength training decreases arthritis pain by 43 percent (!), increases muscle strength and general physical performance, improves the clinical signs and symptoms of the disease, and decreases disability.4 What about dental hygienists - who understand the consequences of poor oral hygiene - “prescribing” hand, wrist, elbow, and shoulder strength training exercises to patients?
Based on his passion for systemic disease and extensive experience with chronically ill patients, Dr. Varon expressed to me his worry about what he perceives to be an oversimplification of some dental diseases, such as periodontal disease, and the various therapies that are used for treatment. He emphasized that oral health care should focus on research outcomes that take into consideration systemic health problems which can greatly affect oral health. This approach makes a lot of sense to me. It’s something we hygienists don’t always think about when we approach older patients with oral care strategies. We need to start looking at the aging boomer population differently. If we see evidence of a sudden or gradual change in oral hygiene that concerns us, let’s begin to think about systemic health problems that perhaps have not yet been diagnosed. Reflect on debilitating conditions like sarcopenia, too, and recognize that loss of body strength has a negative effect on daily living (climbing stairs, cleaning the house, grocery shopping, and oral hygiene care). By developing and applying new tools such as hand assessment instruments for sarcopenia and other systemic health disorders, we will find ourselves renewing our commitment to nutritional and oral hygiene analysis and counseling to patients, families, and caregivers. Let’s think like Dr. Frank, and we’ll start thinking way outside the box.
References
1. U.S. Department of Health and Human Services: Oral health in America: a report of the Secretary General. May 2000.
2. Bross R, et al. Anabolic interventions of aging-associated sarcopenia.
3. J of Clinical Endocrinology and Metabolism 1999; 84(10): 3420-3430.
4. U.S. Department of Agriculture: Low protein + low exercise = sarcopenia. Agricultural Research Magazine, May 2005; 14-16.