A plan for autism: ASD patients can be rewarding experience for dental professionals
By Lisa Dowst-Mayo, RDH, BSDH, and Victoria J. Cabello, RDA, RDH
As a former dental assistant of seven years and now a dental hygienist, I have experienced challenging moments when treating patients with special needs. Prior to entering my dental hygiene program, I had the pleasure of working for Christian C. Cabello, DDS, who taught me many of the tools needed when planning and executing dental procedures for patients with autism spectrum disorder (ASD). I have carried many of these techniques with me into my career.
Dr. Cabello is a diplomat of the American Academy of Pediatric Dentistry and a board member of the Texas Association of Pediatric Dentistry. She has always possessed a natural ability for working with children, especially those with special needs. Dr. Cabello says, "It has always been a passion of mine to work with children because they're so impressionable and a joy to work with. I see all kinds of children, from neuro-typical to cognitively-challenged. In my office, I'm likely to treat one child with autism a day."
This article will present the recent changes to the definition of autism based on the latest edition of the Diagnostic and Statistical Manual (DSM), published in January 2015. Vital statistics, defining characteristics, and dental office management techniques will also be discussed. This article should help improve readers' confidence when treating patients with ASD.
Defining autism
According to the DMS-5, ASD now falls under neurodevelopmental disorders, and Asperger's was removed completely. The DSM-5 defines autism as a disorder "characterized by persistent deficits in social communication and interaction across multiple contexts, including deficits in social reciprocity, nonverbal communicative behaviors used for social interaction, and skills in developing, maintaining, and understanding relationships." Additionally, the diagnosis must also be accompanied by repetitive patterns of behavior, interests, or activities. These anomalies must have clinical distinctions from what is considered "typical" developmental behavior based on type, frequency, and intensity of the behavior in order to avoid a misdiagnosis.1
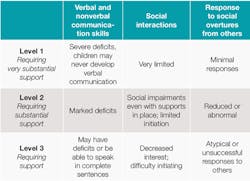
There are varying degrees of severity classified into three different levels (see Table 1).
At all levels of impairment, patients will display an inflexibility in behavior and scheduling. These patients will have difficulty coping with change and express distress when forced to shift their focus from one of their repetitive behaviors. Each patient's language impairment will be different; some will never learn to speak and others will learn to speak fluently and in complete sentences.1
ASD is not a degenerative disorder. Learning, behavior, and compensation will continue throughout their lifetime. Symptoms will be most severe during early childhood, with marked improvements and developmental gains throughout the adolescent years. As adults, those with a lower level of impairment (level 3) may live and work independently if they find their niche of special interest. Adults may suffer from stress, anxiety, or depression and learn to "mask" their difficulties in social settings to maintain a "socially acceptable façade."1
Statistics
The overall prevalence of autism is 1% in the United States,1 or one in 68 children.2 The age and pattern of onset are typically recognized no later than the second year of life. If developmental delays are more severe, recognition is possible during the first year of life.1 However, as the Centers for Disease Control and Prevention reports, most children in the U.S. are diagnosed after age four, with a majority being Caucasian rather than Hispanic or African-American.2 A child may develop typically or "cognitively normally," but then regress during the first two years of life. The DMS-5 reports ASD is diagnosed four times more frequently in males than females.1
According to the 2014 Community Report on Autism, as reported by the CDC, "Almost half of children identified with ASD have average or above average intellectual ability."3 The CDC estimates the annual cost burden to families raising a child with ASD to be $17,000 more than raising a child without ASD. Costs include health care, education, ASD-related therapy, family-coordinated services, and caregiver time. Taken together, it is estimated that total societal costs of caring for children with ASD totaled over $11.5 billion in 2011.3
According to a report published by the American Academy of Pediatrics in 2011, the U.S. has experienced an increase in ASD of 289.5% over the past 12 years.4 There are many theories for this rise in prevalence. The three most common reported in the literature are as follows:5
1. Changes in how prevalence is being measured by surveys and surveillance systems.
2. Changes in ASD awareness, screening tests, access to diagnostic services, diagnostic criteria, and special education placements, that all have led to a more accurate identification of children with ASD.
3. Changes in either ASD genetic susceptibility among persons having children within a population, or nongenetic risk factors.5
Dental management
Dental professionals with little to no experience working with patients who have ASD may feel anxious when interacting with these children. With the reports that the prevalence and incidence of autism is on the rise, the likelihood of a private practice dental professional encountering a patient with ASD is higher than you may think.6 It is important to remember each child will present with varying degrees of developmental coordination disorder (formerly known as sensory integration disorder).1 Therefore, it is vital to organize the appointment to the patient's individual needs. For example, playing a patient's favorite movie or song can help soothe the child. These accommodations should be discussed during planning the appointment with the child's parents.
Short, morning appointments are generally best because this is the time of day when children are most rested and less likely to have experienced a daily stressor.7 Providing a safe and calm environment for a patient with ASD will be beneficial for everyone. Dr. Cabello says, "The less sensory stimulation and stress a child has been exposed to, the more successful the appointment will be. I usually schedule my patients with ASD first thing in the morning because there is less noise and chaos."
The dental provider's word choices are extremely important when working with patients with ASD. These children are very literal and have black-and-white thinking.7 They will not be able to understand inferences or sarcasm1, and they will take the staff's word at face value. So, say what you mean and mean what you say. Use direct commands in a monotone, neutral voice, and avoid fluctuations in your language.
It is best for patients with ASD to work with the same providers and in the same environment because routine is very important to them. After Dr. Cabello gets to know her patients with ASD, she knows what behaviors to expect from them. "I schedule my patients with ASD with the same assistant, and in the same operatory, to help them feel at ease. We also use the tell-show-do technique and follow the same routine every single visit."
The D-Termined program is recommended for dental providers who treat patients with ASD.7 The program consists of five steps-divide the skill into smaller steps, demonstrate the skill, drill the skill, delight the learner, and delegate the repetition.
Table 1
Dr. Cabello said she used this program with Luis at his first visit. "Dividing the main dental goals into smaller steps helped me desensitize Luis to the treatment steps. I allowed him to sit in the chair in intervals-first five seconds, then 30 seconds, and then one minute." To demonstrate drill the skill, she used the tell-show-do technique and had Luis practice it multiple times. She makes patients happy with positive reinforcement. "This encouraged Luis and assured him that his actions and behaviors were favorable. Once he felt confident enough to proceed with actual treatment, we performed what needed to be done. I rewarded his behavior with verbal encouragement and a prize from the treasure box."
Dr. Cabello said she uses sedation or general anesthesia only when appointment goals cannot be reached using the D-Termined program. With level-1 or -2 children, sedation may be the only option for dental treatment as their impairments are more severe than a level-3 child.
Finally, it is important to communicate with the child's team of experts. A child with ASD may be working under the care of many specialists such as a pediatrician, psychologist, psychiatrist, occupational therapist, speech therapist, physical therapist, or neurologist.7Consulting with these providers will allow dental clinicians to fully understand the child's needs and increase confidence in their abilities to provide care.
The occupational therapist or speech therapist may be the most helpful specialists for the dental clinician because they can provide direct information about the patient and explain expectations for dental visits. For example, they may recommend picture cards for communication. When a patient with ASD gets frustrated, they lose their ability to communicate with words and their expressive language becomes dramatically compromised.1
If a trigger is ignited and a meltdown ensues, don't give up on these patients. Try having them sit down and draw a picture, or give them magnetic letters so they can spell out their feelings or communicate their needs. Their frustration may be something as simple as the dental light is too bright, and that is an easy fix. If you just give up and reschedule immediately, you may not be able to get them back.
Treating a patient with ASD can be a rewarding experience for clinicians and families when you use the ideas discussed in this article. Any dental professional can manage a safe and successful dental appointment for patients with ASD by using patience, empathy, compassion, and a predictable environment.
Dr. Cabello reports, "Luis has come a very long way. From waiting two hours in the car because he didn't want to walk into our office, to now being able to sit through a dental procedure with ease, he has made huge improvements. It took a long time, but with patience and a routine, Luis and his mom look forward to visiting my office." RDH
Lisa Dowst-Mayo, RDH, BSDH, graduated magna cum laude with a degree in dental hygiene sciences from Baylor College of Dentistry in 2002. She is currently pursuing a master's in health administration from Ohio University. She is a full-time professor at Concorde Career College in the dental hygiene department where she teaches clinical sciences, board review, special needs, and pharmacology. She is a published author and national speaker and can be contacted through her website at www.lisamayordh.com. Victoria J. Cabello, RDA, RDH, is a native of Laredo, Texas and a current dental hygiene student who possesses an immense passion for dental hygiene, community service, and writing. Prior to entering her academic career, she served as a dental assistant for seven years in the public health sector. Her altruistic nature has led her to volunteer for several organizations including Haven for Hope and Each One Teach One in San Antonio, TX where she resides. An aspiring author and oral health advocate, Victoria plans to obtain a masters degree in public health and continue to expand her writing skills. She also hopes to one day launch new oral health initiatives by starting her own non-profit organization in her community.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorder. 5th ed. 2013. Arlington, VA: American Psychiatric Association.
2. Centers for Disease Control and Prevention. Community report on autism. 2014. Retrieved from http://www.cdc.gov/ncbddd/autism/states/comm_report_autism_2014.pdf.
3. Centers for Disease Control and Prevention. Developmental Disabilities: Key findings: trends in prevalence of developmental disabilities in U.S. children, 1997-2008. 2015. Retrieved from http://www.cdc.gov/ncbddd/developmentaldisabilities/features/birthdefects-dd-keyfindings.html.
4. Boyle C, Boulet S, Schieve L, et al. Trends in prevalence of developmental disabilities in U.S. children, 1997-2008. 2011. Pediatrics, 127(6). doi:10.1542/peds.2010-2989.
5. Schieve L, Rice C, Yeargin-Allsopp M, et al. Parent-reported prevalence of autism spectrum disorders in US-born children: An assessment of changes within birth cohorts from the 2003 to the 2007 National Survey of Children's Health. 2012. Matern Child Health J, 16:S151-S157. doi 10.1007/s10995-012-1004-0.
6. Jolly A. Handle with care: Top ten tips a nurse should know before caring for a hospitalized child with autism spectrum disorder. 2015. Pediatric Nursing, 41(1):11-22.
7. Wilkins E. Clinical Practice of the Dental Hygienist. 10th ed. 2009. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.