The “a-ha!” moments of glycine powder air polishing, with Silky Sharma, EdD, RDH
What you'll learn in this article
- Glycine powder air polishing offers gentle, biocompatible subgingival biofilm removal with proven periodontal health benefits.
- Subgingival glycine air polishing improves efficiency, enhances patient comfort, and supports evidence-based nonsurgical periodontal therapy.
- Dental hygienists integrating glycine air polishing report healthier gingiva, reduced inflammation, and increased patient compliance.
- Air polishing with glycine powder surpasses traditional polishing techniques, creating a modern, research-supported approach to oral hygiene.
- Incorporating GPAP into hygiene appointments elevates clinical care, combining efficiency, comfort, and advanced dental technology benefits.
Silky Sharma, EdD, RDH, is an associate professor teaching senior-level dental hygiene students. Her areas of expertise include periodontology for dental hygiene, pain management, scientific literature, advanced clinical courses, perioscope clinic, and oral pathology.
She’s a a practicing hygienist with a bachelor’s degree in molecular biology and a master's degree with a focus on evidence-based decision-making. Her doctoral work reflects her passion for research and dentistry. During the last four years, she’s spoken nationally and internationally on various platforms about nonsurgical periodontal therapy.
What is your experience with air polishing, both supragingival and subgingival?
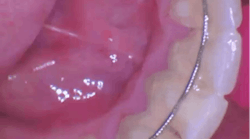
I was introduced to subgingival glycine-based powder about 12 years ago, and I’ve been teaching it ever since. Before that, I regularly used air polishing for supragingival stain removal with sodium bicarbonate, which, as we know, has its limitations. I still use sodium bicarbonate-based air polishing supragingivally for stain removal, but for biofilm removal I now rely on glycine powder air polishing (GPAP) subgingivally.
Comparing subgingival GPAP to motor-driven polishing honestly feels like an insult to technology. What makes GPAP unique is the use of glycine powder to remove subgingival biofilm.
Glycine is an amino acid derivative, which makes it biocompatible, gentle, and highly effective for biofilm removal. This technology enables us to access areas where sodium bicarbonate powder is too harsh or unsuitable.
What were some of your “a-ha!” moments?
When I was introduced to GPAP technology, I dove into the research and found several systematic reviews that supported its effectiveness in removing subgingival biofilm. Once I saw the evidence, I felt confident incorporating it into clinical practice.
Honestly, once I started using it, I fell in love with hygiene all over again. In a clinical setting, time is everything and patient comfort is critical. At the same time, our approach must be grounded in evidence. I like to compare the moment to when I started using loupes with a light. After putting them on, I remember thinking, "Where have I been practicing this whole time … in a tunnel?" A similar eye-opening shift occurred when I began using GPAP. It changed how I practice.
Was there a particular patient you had an “a-ha!” moment with?
I had a perio maintenance patient who couldn’t afford surgery at the time and had generalized 8 mm pockets. Every visit, he presented with heavy biofilm in those deep pockets. It took a tremendous amount of time for his perio therapy. When I integrated GPAP subgingivally, it was significantly more efficient. The technology helped in the removal of most of the biofilm, allowing me to focus on ultrasonics, exploring, hand scaling, and other aspects of supportive perio therapy.
What kind of differences did you notice?
Patients had less gingival inflammation. The gingival description was a lot healthier. The patients were more compliant, and they also felt the difference. It was more comfortable for them.
What have been the “a-ha!” moments for your students?
When we incorporated GPAP into our curriculum, the students immediately noticed the difference. They started using it consistently on their patients, and they liked it so much that I actually had to make some adjustments to the curriculum. I wanted to ensure there was a balanced approach, so students continued practicing hand scaling for plaque debridement strokes.
It was important to me that our graduates left with strong hand instrumentation skills, while knowing how to integrate GPAP and ultrasonics into their clinical care. GPAP and ultrasonics are excellent tools, but they don’t replace hand instrumentation, and there’s no solid evidence to support that they should.
How have you integrated GPAP into your practice clinically?
I start every single patient with GPAP, no exceptions. I begin with the supragingival tip, which, as we know, can effectively remove most of the biofilm in pockets up to 4 mm. After that, I move on to ultrasonics, then explore, hand scale, and re-explore each surface. Honestly, I can’t even remember the last time I used a prophy angle; there’s just no need for it anymore.
Do you face resistance from any patients, students, or colleagues?
Twelve years into using this and I’ve yet to face any real resistance. The only time a patient might seem a bit guarded is if they previously had an unpleasant experience with sodium bicarbonate. When this happens, I take a moment to explain the difference, and once they try it, it’s no longer an issue.
What are the patient considerations posttreatment?
There are no special post-op instructions. Glycine is gentle, nonabrasive, and well tolerated by patients. The use of warm water makes it a great option for patients with dentinal hypersensitivity.
Is there a learning curve with glycine air polishing?
There’s no learning curve at all. For clinicians already familiar with using sodium bicarbonate, the transition is straightforward and requires only a few minor modifications. Adapt the supra tip at a 45-degree angle toward the gingiva, keep it 3 mm to 5 mm away from the tooth, and use a “smiley face” motion for five seconds per tooth. I’ve also shared several videos on my Instagram and in my Facebook group that demonstrate how to use these tips.
Do you see air polishing becoming a standard part of dental practice?
Absolutely. I believe it’s on its way to becoming a standard of care. It’s supported by both evidence and guidelines from our organizations. It improves patient comfort, increases efficiency, and is backed by research as an effective adjunct for biofilm removal.
Where can people find you if they have questions or would like to learn more about this technology?
I offer several hands-on courses on advanced instrumentation that incorporate this technology, as well as several webinars. All that information is available on my website at dantece.com. For more evidence-based content related to nonsurgical periodontal therapy, you can follow me on Instagram @eb_for_nspt and my Facebook group, EB for NSPT.
Editor's note: This article appeared in the August/September 2025 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.