X–ray X–perts
by Bill Landers
[email protected]
X–rays are indispensable diagnostic tools but, being invisible, it's easy to forget that they are one of the three deadliest types of ionizing radiation. Since hygienists use X–rays and are exposed to more of them than dentists, every hygienist should be the office “X–ray X–pert.”
Unfortunately, much of what you learned in school, even if you're a recent grad, is probably out–of–date. Remember röengtens, REMs, and RADs? They haven't been used in the biological literature for years! Here's a refresher.
X–rays were accidentally discovered in 1895 by Wilhelm Röntgen who won the first Nobel Prize in physics for the discovery. He named them “X–rays” because no one knew what they were. X–rays turned out to be identical to gamma rays. They are located on the electromagnetic spectrum just above ultraviolet rays, and you know how dangerous those are. X–rays though, with their shorter wavelengths, are many times more powerful ... so powerful that they can knock electrons off atoms, creating ions (highly charged, highly reactive particles). That's why they're called an ionizing radiation.
X–rays used to be measured in röentgens, a measure of energy equal to the number 208 followed by 109 zeros. That may be useful to physicists, but biologists are more interested in learning what X–rays do to human tissue. The röentgen was eventually replaced with the REM (Röentgen Equivalent in Man), but that's just equal to 1 röentgen multiplied by another big abstract number, the radiation constant (Q).
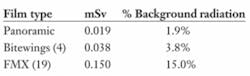
Nowadays, X–rays are measured in comparison to something everyone can envisage, the annual, natural background radiation that we get from galactic gamma rays and radioactive isotopes in the earth. The new international measurement unit is the millisievert (mSv), which makes it easy to understand relative radiation risks. For instance, a panoramic film = 0.019 mSv, or 1.9% of the total background radiation that an average American gets in one year (excluding radon). Similarly, one set of four bitewings = 0.038 mSv or 3.8% of the natural background radiation and a full–mouth series (19 films) = 0.150 mSv or 15% of the average annual natural dose. But it's important to remember that it really isn't 15% “of” the annual background radiation. It's 15% more than the average annual dose. A full–mouth series adds 15% to one's total annual radiation dose.
Hygienists are exposed to more radiation than the average person, but the extra ionizing radiation doesn't come from the X–ray machine. It comes from the patient in the form of scatter (not scattered) radiation. Scatter radiation isn't composed of X–rays reflected from the patient. Most of the machine–generated X–rays are either absorbed by the patient's tissue or pass straight through to the film. However, about one–third of the original, primary X–rays collide with atoms in their path, knocking off electrons. Like a miniature nuclear reaction, those electrons get absorbed by nearby atoms. The extra energy gets released in the form of a brand new X–ray, which can shoot off in any direction including back toward the operator.
Scatter X–rays don't make it very far though. Their density falls off with the square of the distance. That means that the number of X–rays three feet from the patient will only be 1/9 of the X–rays one foot away. The more distance and dense things (like a lead barrier) between the operator and the patient, the less scatter radiation received. Even with precautions, the operator still receives some radiation. It's very, very small, but not quite zero. Fortunately, you can receive many times the average natural background dose safely. The annual X–ray limit for health–care workers is 20 mSv a year (20 times the average annual background radiation).
Now you're an “X–pert”!
Bill Landers has been president of OraTec Corp. since 1992. He is also a leading expert on chairside and laboratory periodontal risk assessment technologies, and his essays on periodontal disease have been published in several dental hygiene journals. Landers is a popular speaker and has presented hundreds of continuing education seminars on the microbiology of periodontal diseases.