When William and Katie were young, I used to read to them every night, come what may. I remember repeating the famous line in Goldilocks fairy tale where the great big bear looks at his bed and cries out: “Who's been lying on my bed?” When we use a disclosing solution and show our patients plaque/biofilm, start out by saying something like, “Look who's been living on your tooth!” and perhaps you'll engage the patient in conversation about something other than the weather.
Last month, I introduced a new metaphor, something a bit corny but designed to get patients to pay attention to your message about suppressing biofilm communities. Just as your significant other may not be paying attention to you because he or she is instant messaging someone, so do your patients also tune you out. If you start discussing biofilm as a community of slugs, either your patients will think you belong in a loony bin or they might just sit up and take notice.
I'd like to challenge companies who make disclosing solutions to create a nice, colorful 8” x 11” laminated poster which illustrates stained biofilm on teeth and a second image that shows some biofilm organisms attached to a tooth surface that actually resemble little people. I have a lot of fun with biofilm images and when I show them to patients, it's an opportunity to tell a lot of stories. For example, ask your patients if they have ever observed pink stains (pink biofilm) on wet surfaces in their bathrooms, like in sinks or showerheads. Don't tell them that they have showerhead slime on their teeth, but find ways to make the metaphor stick. We've all seen children and even adults with biofilms on anterior teeth in shades of yellow, brown, orange, green, and even salmon!
Like slugs, biofilms use their extracellular polymeric substance (or gooey slime called EPS) as an armor against the enemy.1 I used to think it was impossible for periodontal pathogens to travel from the mouth to different parts of the body because I knew that packs of wolves (neutrophils and macrophages) would engulf them. Now I understand that detachment fragments or “packets” of bacterial cells can slough off and travel to unknown destinations.
I didn't realize the tremendous protection offered to bacteria in their travels around the body by EPS material. Like voyages of a shielded Starship Enterprise, pathogens are safely encased and protected against the host defense system. In my mind, I sometime envision these fragments initiating clots in blood vessels, making atherosclerotic plaques more dangerous. I also wonder about the volume of aspirated and EPS-protected anaerobes that can colonize a patient's airways and contribute to anaerobic/aspiration (nosocomial) pneumonia. By the way, endotrachael tubes also colonize biofilm, and I never used to think about that either. As the American population continues to age, our profession will be armed and ready to enter hospitals and other institutions as frontline providers to prevent and eliminate oral biofilm infections, once barriers imposed on us by state practice acts are lifted.
We still have a lot to learn about biofilm communities because it wasn't until 1978 that researchers discovered them as the predominant means of bacterial growth in virtually every natural environment. As we continue to learn more about ways to suppress biofilm and barriers to host healing, protocols for the prevention and treatment of oral infections will continue to be modified. In the meantime, we can learn a lot from medical providers who are now specializing in biofilm-based wound management. Wound healing, like periodontal pocket wound healing, is complex and there's still a lot we don't know about the biochemical and cellular aspects of wound repair and biofilm and host/biofilm interactions.2
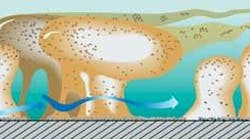
For many years, the medical literature referred to slough on the surface of wounds as dead host tissue that, when removed, re-grows again quickly. It's been described as a living organism growing on the surface of a wound. Does this sound like biofilm? Yes, indeed! As microscopic evaluation continued, it became apparent that chronic wound beds are loaded with biofilm and that biofilm uses capillary and venular walls as the preferred surface to spread deep into the wound. Like periodontal pocket environments, chronic wounds don't heal well unless biofilm is adequately suppressed.
Wound experts are now finding new ways to suppress biofilm to promote wound healing, just as we teach our patients to use multiple concurrent strategies to manage oral biofilm.We can learn from wound experts and they can continue to learn from us, too. Wounds are a serious problem worldwide and account for an overwhelming portion of health-care costs in the United States.2 In wound therapy, “debridement of the wound is the central point around which all other elements of wound care must revolve.”2
Can we make the same point about non-surgical periodontal therapy too? Even in other industries that face biofilm challenges, mechanical cleansing is done, followed by the use of oxidative biocides to kill sessile and planktonic cells. That's essentially what we do as therapists when we debride (clean) and disinfect pockets with topically or locally delivered antimicrobials.
Biofilm-based wound care recognizes the importance of shaping the wound to favor the host, not the biofilm. Biofilm organisms love deep, moist periodontal pockets and calculus and they adore tunnels, tracks and redundant folds of tissue in chronic wounds. Sometimes wound experts, like periodontists, change the architecture to favor the host through various surgical procedures. Wound experts have also discovered that, in impaired hosts, biofilm tends to be faster growing too.2
One goal of wound care experts is to create a wound bed that is not only free of biofilm but free of necrotic material, which is described as granular and red in appearance.2 How many times do most clinicians scale subgingivally (blindly, I might add) in a deep pocket and remove red, necrotic tissue without disinfecting the pocket afterwards and re-evaluating it for healing? The point here is that, at the time of re-evaluation, if bleeding persists, we know that biofilm is still present in the pocket. You cannot allow this area to go untreated for another six months or more!
In chronic wound management, the usefulness of systemic antibiotics is controversial and their use has been generally discouraged.2,3 If the goal is a wound bed with suppressed biofilm, the protocols include multiple concurrent strategies. If antibiotics are used, they are now used based on current sensitivity testing in high doses for longer periods of time and in conjunction with other strategies like debridement, various biofilm agents like xylitol, biocides, and anti-biofilm dressings. In a future column, I will focus on new biofilm agents and research that is being done to find new ways to combat medical and oral biofilms.
While scaling to remove subgingival calculus deposits with the aid of a periodontal endoscope, you can see the billowing biofilm cloud that is attached to the calculus. Years ago, wound experts used to think that the “slough” that sat on top of chronic wounds was inconsequential, too, but, to everyone's astonishment, this is a powerful force to be reckoned with and a huge deterrent to chronic wound healing.
References:
1. http://www.biofilm.montana.edu/Res-Lib99-SW/newsarchives/HTML/2007/Program%20Abstract%20Book.pdf
2. http://www.woundcarecenter.net
3. http://www.cochrane.org/reviews/en/ab003557.html
About the Author
Lynne Slim, RDH, BSDH, MSDH, is an award-winning writer who has published extensively in dental/dental hygiene journals. Lynne is the CEO of Perio C Dent, a dental practice management company that specializes in the incorporation of conservative periodontal therapy into the hygiene department of dental practices. Lynne is also the owner and moderator of the periotherapist yahoo group: www.yahoogroups.com/group/periotherapist. In addition, Lynne is the editor of the Sunstar Americas e-newsletter “The GUMline.” Lynne speaks on the topic of conservative periodontal therapy and other dental hygiene-related topics. she can be reached at [email protected] or www.periocdent.com.