7,680 times a day: Are you protected from the risk of invisible dangers?
Droplet transmission
A person’s respiratory rate is the number of breaths the person takes per minute. The normal respiration rate for an adult at rest is 12 to 20 breaths per minute.1 In an eight-hour workday, the average number of respirations is 7,680. Are you protected from potential bioaerosol risk during patient care and infection control–related activities, such as instrument reprocessing and turning of a treatment room?
Some diseases can be transferred by infected droplets contacting surfaces of the eye, nose, or mouth. This is referred to as droplet contact transmission.
In health-care settings, encouraging good health habits such as proper respiratory hygiene with Cover your cough from the Centers for Disease Control and Prevention, and frequent handwashing implemented at the first point of contact can often help stop the spread of germs and prevent respiratory illnesses such as flu.2
The following measures are recommended for all individuals with signs and symptoms of a respiratory infection to contain respiratory secretions.
- Cover mouth and nose with a tissue when coughing or sneezing. Use the nearest waste receptacle to dispose of tissue after use.
- Perform hand hygiene (e.g., hand washing with nonantimicrobial soap and water, alcohol-based hand rub, or antiseptic handwash) after having contact with respiratory secretions and contaminated objects and materials.
- Provide tissues and no-touch receptacles for used tissue disposal.
- Provide conveniently located dispensers of alcohol-based hand rub. Where sinks are available, ensure that hand washing supplies (i.e., soap, disposable towels) are consistently available.
Water and bioaerosols are everywhere
Patients and staff are exposed to microorganisms from dental unit water-line water and to bioaereosols generated by dynamic dental instruments, such as ultrasonic scalers, air polishers, handpieces, and air water syringes. In a 2004 literature review by Harrel and Molinari, the ultrasonic scaler (magnetostrictive or piezo) was identified as the greatest source of aerosol contamination due to the composition of particles of varying size, ranging from 0.001 to 100 µm, including both aerosol and spatter.3 Furthermore, dental aerosols can travel up to four feet from the work zone4 and remain airborne for up to 30 minutes, placing the dental team at risk for the transmission of infection.5
Every water exchange, or the aerosols generated by the equipment, is a potential exposure to the opportunistic waterborne microorganisms, including Legionella, Pseudomonas, and Mycobacterium, which can survive and thrive in complex dental unit tubing. Bioaerosol compositions are heterogeneous—they contain blood, microorganisms, mucosal cells, restorative materials, tooth particles, and large quantities of saliva.6
Studies have shown that chronic exposure to these bioaerosols may be a risk factor for cross-infection for dental health professionals. The results from a 1985 study done on the incidence of respiratory disease in dental hygienists indicate they have a 60% higher incidence of cold symptoms than a similar professional group without dental patient contact.7
It has been well documented that the most likely mode of disease transmission in dentistry is through inhalation of bacterial aerosols or spatters. Ninety-five percent of dental aerosols are 5.0 µm or less in diameter and cannot be seen.8 Microorganisms isolated from these particles include staphylococci, pneumococci, tubercle bacilli, influenza viruses, hepatitis viruses, rhinoviruses, and herpes viruses.
The most effective means to reduce the risk of droplet transmission of pathogenic organisms and other potentially infectious materials (OPIM) is the appropriate selection and correct use of personal protective equipment (PPE), such as gloves, masks, eye protection, and face shields.
Up in smoke
With laser dentistry on the rise, dental professionals are facing a new set of occupational health risks—the potential transmission of disease through the laser plume.9 Ninety-five percent of laser plume is made up of water, but the remaining 5% contains potentially hazardous bioaerosols, including cellular debris, blood fragments, and bacteria.9
To prevent contact with splashes, spatter, and plume, dental health-care personnel should position patients properly and make appropriate use of barriers (e.g., face shields, protective eyewear, high-filtration masks, and gowns), rubber dams, and high-volume evacuators.
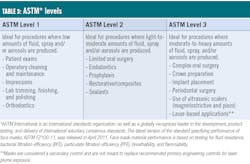
Select the mask for the task (tables 1–3)
The key to choosing the right mask for the task lies in three areas: quality of material and manufacturing, design with custom fit, and whether it’s compliant. In addition, it’s important to understand mask ratings in order to choose the appropriate mask protection level for each procedure performed in the practice. Several mask designs are considered to provide exceptional comfort.
The Ultra-Sensitive ear loop mask with secure fit technology from Crosstex, for example, has a white hypoallergenic, extra soft inner cellulose layer. It will not lint, tear, or shred.
Masks with flat ear loops attached to the outside of the mask (as opposed to the inside of the mask) provide a comfortable fit and help eliminate irritation.
Masks free of latex, fiberglass, chemicals, inks, and dyes help minimize skin sensitivities.
Masks with antifog or fog-free strips on the inner layer block and absorb moisture. They also form a strong seal, preventing eyewear from fogging while they cushion the nose ridge.
Some masks have unique vapor barriers on the outside layer, further blocking moisture.
Crosstex masks with Secure Fit mask technology feature flexible aluminum strips above the nose and below the chin, which creates additional breathing space and allows for a custom fit, regardless of face shape or size. This innovative design significantly reduces gapping at the top, bottom, and sides, which increases the effectiveness of mask protection. Even if a mask has a high-level filter, the lack of a close circumferential seal to the face will negate filter performance because particles will follow the path of least resistance and travel through the gaps between the mask and face. Most regulatory and professional organizations recognize the inherent fit issues of masks showing gaps along the cheeks and chin. A recent study evaluating the total leakage through a surgical face mask indicated 5%–8% came from filter leakage, and 25%–38% came from face seal leakage.6
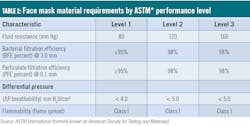
ASTM International is an international standards organization, as well as a globally recognized leader in the development, product testing, and delivery of international voluntary consensus standards. The latest version of the standard specifying performance of face masks, ASTM F2100-11, was released in April 2011. Face mask material performance is based on testing for fluid resistance, bacterial filtration efficiency (BFE), particulate filtration efficiency (PFE), breathability, and flammability.
Donning
- Proper preparation and placement of the mask impacts the ability to protect the dental health professional (DHP) from bioaerosols and particles.
- Only the exterior layer is fluid resistant—know the front versus the back. The side facing up in the product box is always the front exterior of the mask.
- Prior to placing the mask to the face, create a concave divot with your thumb in the aluminum noseband to guide for proper placement high on the bridge of the nose. Slightly extend the face mask by pulling the chin-side edge down.
- Pleat configuration should be open in a downward “waterfall” effect to prevent pooling of condensate or aerosols that will result in wicking or soak-through of microbial-laden fluids into direct contact with the nose and lips from the lining layer.
- Holding mask by the ear loops, orient the noseband divot placement on the face and secure a loop around each ear.
- Never twist the ear loop into a figure eight to gain a closer fit as this will cause the inner lining of the mask material to be in close contact with the lips and nose, which leads to increased moisture from condensation and increased risk of contamination through the layers of material. Consider a mask designed with an additional malleable chin-strip to provide a more secure 360-degree comfort fit.
- Mold the nosepiece with index and middle finger for a secure fit across the bridge of the nose and along orbits of the eyes.
- Never pinch the noseband with thumb and index finger as v-notch exposure will remain in the greatest area of contamination of the face—across the bridge of the nose and between the eyes.
- Fully extend the chin-edge of the mask to cover the mouth and chin.
- If an additional malleable chin-strip is available, pinch it snugly and directly under the chin to create a 360-degree peripheral seal.
- Masks are single-use disposable and must be changed with every patient. Additionally, masks have a use-life. Best practice dictates changing a mask if the fluid-resistant outer layer becomes wet or soiled with exposure to spatter or bioaerosols or the internal lining layer becomes moist from breath condensation. Masks should be changed every 20 minutes in an aerosol environment and every 60 minutes in a nonaerosol environment during lengthy procedures.10
Bottom line
Are you choosing and using the best mask to be protected from the risk of invisible dangers?
References
1. Vital signs. Cleveland Clinic website. https://my.clevelandclinic.org/health/articles/10881-vital-signs. Reviewed January 23, 2019. Accessed September 20, 2019.
2. Respiratory hygiene/cough etiquette in healthcare settings. Centers for Disease Control and Prevention website. https://www.cdc.gov/flu/professionals/infectioncontrol/resphygiene.htm. Reviewed August 9, 2009. Accessed September 20, 2019.
3. Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135(4):429-437.
4. Veena HR, Mahantesha S, Joseph PA, Patil SR, Patil SH. Dissemination of aerosol and splatter during ultrasonic scaling: a pilot study. J Infect Public Health. 2015;8(3):260-265.
5. Harrel SK. Contaminated dental aerosols: The risks and implications for dental hygienists. Dimensions of Dental Hygiene. 2003;6:16-20.
6. Kobza J, Pastuszka JS, Bragoszewska E. Do exposures to aerosols pose a risk to dental professionals? Occupational Medicine. 2018;68(7):454-458. Published June 20, 2018. Accessed September 20, 2019.
7. Rosen S, Schmakel D, Schoener M. Incidence of respiratory disease in dental hygienists and dietitians. Clin Prev Dent. 1985;7(5):24-25.
8. Molinari J, Nelson P. Face mask performance: Are you protected? Oral Health Group website. https://www.oralhealthgroup.com/features/face-mask-performance-protected/. Published March 16, 2016. Accessed September 20, 2019.
9. Ulmer BC. The hazards of surgical smoke. AORN J. 2008;87(4):721-734.
10. Jorgenson G, Palenik C. Selection and use of personal equipment. The Dental Assistant. 2004;73:16-19.
With more than 20 years of academic and directorial experience, LEANN KEEFER, MSM, RDH, has a reputation as a trailblazer and is an international speaker in infection prevention. In her role as director of clinical services and education for Crosstex International, Keefer identifies trends in health care and infection prevention, developing and implementing the company’s strategies relating to education and professional relations. Keefer was appointed to the OSAP Association Board of Directors in 2012 and serves on various foundation and publication boards in the US and Canada.
About the Author

Leann Keefer, MSM, RDH
With more than 20 years of academic and directorial experience, LEANN KEEFER, MSM, RDH, has a reputation as a trailblazer and is an international speaker in infection prevention. In her role as director of clinical services and education for Crosstex International, Keefer identifies trends in health care and infection prevention, developing and implementing the company’s strategies relating to education and professional relations. Keefer was appointed to the OSAP Association Board of Directors in 2012 and serves on various foundation and publication boards in the US and Canada.