Overcoming anesthesia failure: Increasing your odds of success with the IA block
Dental hygienists often rely on the traditional inferior alveolar nerve block (IANB), also known as the Halsted approach, plus the addition of the buccal block for mandibular quadrant anesthesia during nonsurgical periodontal therapy (NSPT). This injection duo is the approach most often taught to clinical competency by dental hygiene education programs, so it is what many of us are used to and feel most confident using. A 2014 study revealed that less than 20% of dental hygiene education programs require students to demonstrate clinical competency for the Gow-Gates mandibular block technique, which is the next most popular mandibular block technique practiced during dental hygiene education.1
The IANB anesthetizes (on one side) the inferior alveolar (IA) nerve, mental nerve, incisive nerve, and lingual nerve. Structures anesthetized include: the pulps of the mandibular teeth; the associated lingual tissues and periosteum; and the facial soft tissues and periosteum of the mandibular teeth anterior to the mental foramen. The anterior two-thirds of the tongue, floor of the mouth, body of the mandible, and inferior portion of the ramus are also anesthetized. The buccal block injection is required to anesthetize the facial soft tissue in the molar region.2-4
The problem with the traditional IANB is the high failure rate. Anesthetizing the adult mandible is more challenging than the maxilla due to the thick cortical bone, especially in the posterior region; unreliable location of landmarks and nerves (which are often asymmetrical on individual patients); potential for accessory innervation; and the depth of soft-tissue penetration required to reach the target.2-5 Careful review of the basic technique for providing the IANB is the first step in increasing one's success rate.
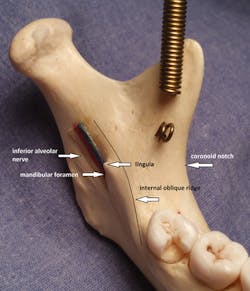
Figure 1: Landmarks, mandible, left side.
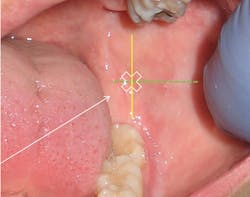
Figure 2: Palpating the coronoid notch, right side.
Figure 3: Example of a position of the mandibular foramen relative to lingula, right side.
Figure 4: Mandible, left side; insertion site. Intersection of horizontal green line drawn from coronoid notch to the pterygomandibular raphe (PMR) and the vertical yellow line drawn three-quarters of the distance from the coronoid notch to the PMR.
Review the anatomy
Dust off your old skull from hygiene school. If you don't own one, consider buying one. This is particularly essential for hands-on learners. I bought my first one several years ago when I began making my own images for CE courses. I bring it on-site so that participants can see and feel the anatomy as I talk about the injections. The anatomically correct, 3-D skull is so much more helpful for feeling anatomy and practicing angulation than looking at pictures alone. Decent skulls can be purchased for about $100. Explain to the manufacturer that you need a skull that accurately reflects the important landmarks (lingula, mandibular foramen, internal oblique ridge, mental foramen, etc). Next, find your head-and-neck anatomy textbook, and together with the skull begin to locate important landmarks. Although it is true that the location of the lingula varies quite a bit, note how it is positioned relative to the mandibular foramen, and practice placing your thumb/finger at the coronoid notch and palpating the internal oblique ridge (see Figures 1, 2).
The target for deposition is the IA nerve after it exits the foramen ovale but before it enters the mandibular foramen. Note that the mandibular foramen is partially covered by the often-elusive lingula ("little tongue") (see Figure 3). Deposition must be within 1 mm of the target for effective anesthesia.
The insertion site is determined by the intersection of two imaginary lines (see Figure 4):
• Height: Imaginary horizontal line from coronoid notch to pterygomandibular raphe (PMR) approximately 6-10 mm superior and parallel to the mandibular occlusal plane.
• Anteroposterior (front-to-back): Imaginary vertical line three-quarters of the distance from the coronoid notch to the PMR.2 Some experts report the vertical line should be two-thirds of the distance.3
Figure 5: Early bone contact; after partial withdrawal; direct barrel more anteriorly.
Figure 7: Left side; palpate inner ridge (black dashed line) with nondominant finger; slide it posteriorly until ridge "disappears"; insert just over the top of that point (white X); angle and advance per traditional IANB. Slashed blue circle represents insertion site of traditional IANB.
Review the basic technique:
Textbooks are very useful, especially for reviewing the details of anatomical features and technique. Your local anesthesia textbook can be a guide or you can buy a more current one, new or used, online. Used textbooks of the most current editions that I have purchased online have always been in excellent condition. I took a look at my original local anesthesia textbook from 1979 to compare the technique from that era to what is recommended currently (see Table 1). The biggest changes I identified were:
1. It is no longer recommended to deposit drops of anesthetic ahead of the needle along the way to the target. 2. An aspiration test should be performed in two or three planes, not just one. 3. There is usually no need to provide a separate injection for the lingual nerve during withdrawal, as the lingual nerve is usually anesthetized from deposition at the target.
Of course, authors have differing views, but with regard to the Halstad approach, they seem pretty consistent.
Tips and tricks
There are probably as many approaches to the IANB as there are clinicians. Described below are a few suggestions for correcting errors and avoiding insufficient anesthesia during provision of the IANB for NSPT.
1. Deposition too low (below mandibular foramen) is the most common error and the most common cause of failure. To correct, reinsert 5-10 mm superior to the original injection site. Many years ago, when I was working at a periodontal office in Milpitas, California, an endodontist showed me a technique that improved my success rate: palpate the internal oblique ridge with a nondominant finger and follow it superiorly. The insertion site is directly over the finger at the point where the internal oblique ridge is no longer palpable. Using this approach, the anesthetic is deposited higher (see Figure 7), above the target area of the traditional IANB and below the target for the Gow-Gates technique.
2. Accessory innervation-Inadequate anesthesia of the mesial portion of the mandibular first molar may result due to accessory innervation, which many experts suggest is likely due to lack of anesthesia to the mylohyoid nerve. Solutions have included providing (1) the mylohyoid nerve block,4 (2) PDL injections, or the (3) Gow-Gates or Vazirani-Akinosi nerve blocks. However, recent studies have shown that a supplemental buccal supraperiosteal injection at the apex of the mandibular first molar using half a cartridge of 4% articaine increases the effectiveness of the IANB.6-8 The success may be augmented through the use of buffered articaine.7
Inadequate anesthesia of anterior teeth may result due to incisive nerve crossover. Providing the incisive block on contralateral side has been shown to be a good remedy.9 For the purposes of NSPT, adequate lingual anesthesia (not provided by incisive block) can be easily achieved in limited areas by providing interpapillary infiltrations at the mesial and distal aspects of the teeth affected.2 The infiltrations should be comfortable for the patient because the facial tissues will already be anesthetized by the incisive block. Alternatives include the administration of supraperiosteal injections or PDL injections.
3. Bifid IA nerve-In less than 1% of the population,3 a bifid IA nerve may be present and may result in inadequate anesthesia. Often a second, more inferiorly positioned mandibular canal is visible on the radiograph. Solutions include depositing local anesthetic more inferior to traditional landmarks, administering supraperiosteal injections on buccal and lingual of teeth affected, or administration of PDL injections.
4. Additional strategies-Studies have shown that the use of buffered local anesthetic results in a more comfortable injection and more rapid onset;10 that articaine is safe and more successful in producing anesthesia than lidocaine for infiltration and blocks;7 and that positioning the patient upright after the injection facilitates diffusion of the local anesthetic in the area.3
Technique protocols, recommendations for agents, and armamentarium evolve. Frequent review of evidence-based approaches to providing mandibular anesthesia is essential for safe and effective pain control. RDH
References
1. Webb L. Best practices in local anesthesia teaching methodology for dental hygiene education. Victoria, BC Canada: CDHA National Conference poster sessions; October 2015.
2. Malamed S. Handbook of Local Anesthesia. 6th ed. St. Louis, MO: Elsevier; 2013.
3. Logothetis DD. Local Anesthesia for the Dental Hygienist. 2nd ed. St. Louis, MO: Elsevier; 2017.
4. Bassett B, DiMarco A, Naughton D. Local Anesthesia for Dental Professionals. New York, NY: Pearson; 2010.
5. Malamed S. Is the mandibular block passé? JADA. 2011;142(9 suppl):3S-7S.
6. Meechum JG. The use of mandibular infiltration anesthetic technique in adults. JADA. 2011;142(9suppl): 19S-24S.
7. Malamed S. Articaine 30 years later. Oral Health. http://www.oralhealthgroup.com/features/1003919408/ Published February 4, 2016. Accessed April 15, 2016.
8. Kanaa JM, Whitworth JM, Corbett IP, Meechan JG. Articaine buccal infiltration enhances the effectiveness of lidocaine inferior alveolar nerve block. Int Endodont J. 2009;42:238-246.
9. Webb L. Investigating the incisive block. RDH. 2015;35(9):94-96.
10. Malamed S, Tavana S, Falkal M. Faster onset and more comfortable injection with alkalinized 2% lidocaine 1:100,000 epinephrine. Compendium of Dental Education-Aegis. 2013;34(1):10-20.
LAURA J. WEBB, RDH, MS, CDA, is an experienced clinician, educator, and speaker who founded LJW Education Services (ljweduserv.com). She provides educational methodology courses and accreditation consulting services for allied dental education programs and CE courses for clinicians. Laura frequently speaks on the topics of local anesthesia and nonsurgical periodontal instrumentation. She was the recipient of the 2012 ADHA Alfred C. Fones Award. She may be contacted at [email protected].
About the Author

Laura J. Webb, MS, RDH, FAADH
Laura J. Webb, MS, RDH, FAADH, is an experienced clinician, educator, and speaker who founded LJW Education Services (ljweduserv.com). She has provided educational methodology courses and accreditation consulting services for allied dental education programs and CE courses for clinicians. Laura has frequently spoken on the topics of local anesthesia and nonsurgical periodontal instrumentation. She was the recipient of the 2012 ADHA Alfred C. Fones Award. Laura can be reached at [email protected].
Updated May 2023